Potential risks to physical safety in the workplace are often easy to identify. However, potential psychological hazards aren’t always as easy to spot, yet can cause just as much harm to a person who is impacted by them.
As an employer, you have a duty to protect your employees from risks to their health, including psychological health. It’s important to note that every jurisdiction has different laws and regulations about psychological safety. Your obligations as an employer will be shaped by the rules that apply to you, however much of the guidance available is useful for employers as best practice even where it is not mandatory.
What are psychosocial hazards?
A psychosocial hazard is a hazard that arises from, or relates to,
- the design or management of work,
- a work environment,
- plant at a workplace, or
- workplace interactions and behaviours
and has the potential to cause psychological harm or injury (Work Health and Safety Regulations 2011 (Cth) section 55A).
Depending on the nature of the workplace, some psychosocial hazards may always be present, while others may temporarily arise due to some change in working conditions. For example, the risk of emotional trauma connected to the loss of a patient in aged care is high and ever-present due to the nature of the work, whereas a psychosocial hazard connected to working increased hours due to staff shortages because of illness is likely to be temporary in nature. In many cases, one or more hazards will interact, and the effects compound to create a greater risk of harm.
Types of psychosocial hazard
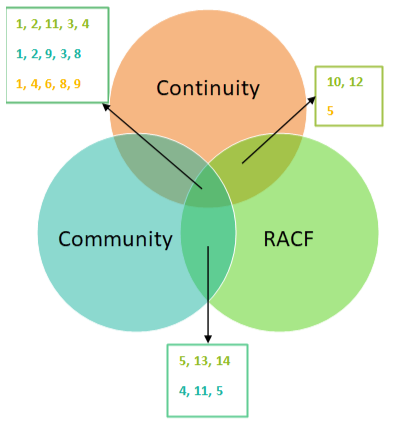
There are three broad categories of psychosocial hazards that employers must manage:
- The working environment – includes hazards such as working in high risk areas, working in remote or isolated areas or working unusual shift patterns.
- The work itself – does the work require unusually high or low levels of mental load, does the work involve exposure to traumatic events or material, and is the workload unreasonably high?
- Interpersonal conflicts – including between staff, poor management of the workforce, or mistreatment of staff by consumers.
Personal issues faced by staff outside the working environment may compound their risk of psychological harm. While employers can’t control these hazards, they may be able to work with staff to ensure that the workplace does not contribute to the staff member’s risk of psychological injury.
Appendix A of the model Code of Practice – Managing psychosocial hazards at work 2022 (Cth) provides a detailed example list of common psychosocial hazards, and potential control measures for each.
What is the current legislative status?
Most states and territories have implemented the model Work Health and Safety laws. As of April 1 2023, some jurisdictions have updated their Work Health and Safety Regulations and introduced a Code of Practice to specifically cover psychological safety and psychosocial hazards. Victoria’s psychological safety falls under its Occupational Health and Safety Act, and reforms are currently underway to better incorporate psychological safety into the existing occupational health and safety regulations.
See the below table for a brief summary of the psychological safety legislative requirements per jurisdiction, or refer to Safe Work Australia for more detailed information.

What do I have to do to manage psychosocial hazards?
In all jurisdictions, employers have a duty to ensure the health and safety of their workers where “reasonably practicable”. This includes considering:
- whether the hazard was reasonably foreseeable;
- the potential severity of the harm that could occur;
- whether the organisation or its management knew or should have known about the hazard;
- whether there are any available and suitable methods of controlling the risk from the hazard; and
- the cost of managing the risk.
Other benefits of good psychological safety
In addition to making sure you’re meeting your legal obligations, good management of psychosocial risks can flow on to benefit the organisation.
Demonstrating care for the wellbeing of employees and making work a mentally healthy place can boost staff retention rates, while staff who aren’t affected by psychological injury are less likely to require time off work, leading to more predictable and consistent rostering.
Checking in with the workforce about psychological health can aid the organisation in understanding the challenges and difficulties staff are facing, while reviewing policies and processes for psychological safety can lead to operational changes improving service delivery.
How SPP can help
We’ve updated these resources for you, which are available in SPP’s Reading Room:
- Info Sheet: Psychological Safety in the Workplace
- Policy: Psychological Safety for Staff
Ready to improve psychological safety?
Sign up to SPP and see how our resources can help you become a psychologically safe workplace!